Author: Alex Lukey, Women's Health Blog Co-Coordinator | Editors: Arrthy Thayaparan, Women's Health Blog Co-Coordinator
Published: April 7th, 2021
This past year will go down in history as the year the world halted at the hands of a global pandemic. But the sacrifice and dedication from our frontline workers, kept hopes up and fears at bay throughout these unprecedented times. For World Health Day, our blog co-coordinator Alex Lukey sat down with two nurses, Krista Koenig and Lauren Dyck, working on the frontlines of COVID-19 hospital floors to talk about the past year.
The Beginning
Alex: Take me back to this time last year. What were those first few months like for you?
Krista: The first few weeks were kind of chaos. Nobody was sleeping well. We were all on edge, trying to figure out what was going to happen.
Lauren: I remember thinking to myself, I've only been out of school for two years. How do I deal with this? Even the people supporting us didn't know what to do, so it was very confusing and scary.
Lauren: Every time we discharged a patient, another one would come through the door. It's kind of what it is like right now actually too. Last spring, we were never over capacity, but we are now. We've got a couple of variants on my unit, and now it’s younger people coming in. Really, really sick people, so it's a lot to deal with for sure. We're all so burnt out trying to deal with the workload and then trying to deal with the deaths on top of it too.
The Hardest Part
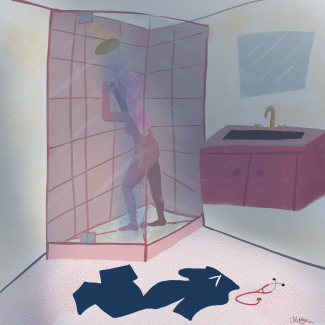
Krista: I've never had trouble sleeping before this. That's kind of where it translated for me. I didn't see my family. I was just so scared of bringing it to somebody that I loved. Even though my family all lives here in town, I couldn't see them.
Lauren: The mental health aspect of not for myself but for the patients. A lot of them, when they come to the hospital and are that sick, they're here for a good three weeks.
Both Lauren and Krista spoke about the difficulty of supporting patients near the end of their lives. While many of the sickest COVID-19 patients are cared for in the intensive care unit (ICU), many long-term care home residents do not go to the ICU. These older adults may choose to forgo life-saving measures such as intubation. So, while nurses in the ICU dealt with many deaths from COVID-19, the brunt of deaths from long-term care homes fell on the shoulders of nurses working on lower acuity COVID-19 units, such as Lauren and Krista.
Lauren: There’s a lot of struggling at the end because you can't breathe. At the beginning, we weren't even allowed visitors for people who were dying, so we'd have to zoom with their families. We would have to help them say goodbye like that which is just horrible. Now we do visits for some people, but some families are scared to come in, which I understand. But you can't fix that emotional part of it. It’s hard to feel like you can't really do anything about it.
Krista: Family members haven't been able to visit unless somebody is critically ill or near death. I think that's been one of the most significant changes for me too. In my practice, it's so much centered around family care and including everybody.
Who is Caring?
Despite personal protective equipment (PPE), nurses are at a high risk of contracting the virus on the job. A report published by BC Women’s Foundation found that 80% of people working in healthcare are women in BC. Further, the roles with the highest risk of exposure due to close physical contact are professions that have higher numbers of women, such as nurses and personal care aides.
Krista: We did have nurses end up testing positive on our floors. We were nursing our own nurses.
COVID-19 also presented women starting families with a difficult decision. While there is much more research needed, there was almost no information on the risks of COVID-19 for pregnant women a year ago. This lack of data continues to be a cause of significant concern for women.
Krista: We have so many pregnant nurses that we were trying to protect. We have such a strong solid group that we just try to look out for each other. We tried to give the positive patients to younger healthy nurses.
Hope
Both Krista and Lauren spoke about how access to the vaccine is giving them hope for the future.
Krista: It’s a big moment for science and history for everyone. Unfortunately, there's still so much fear and miscommunication in this information and media right now about vaccines, but for our group that was such a turning point.
Lauren: When I got vaccinated, it was a very emotional moment for me. I actually almost cried because I was thinking, we're gonna get through this. It's almost like a race right now with our numbers going up and trying to vaccinate as many people as possible.
Meet the Nurses
Krista Koenig
Cardiac Medical RN
Asthmatic Frontline Worker
Vaccinated

Lauren Dyck
Lauren grew up in Vernon, BC, and completed her nursing degree at UBCO in Kelowna in 2018. After graduating, she moved to Vancouver and has since been working at Richmond Hospital on a cardiac/covid-19 ward. She will be starting a new job in May on the cardiac unit at Vancouver General Hospital. She hopes to pursue travel/ER nursing in the future.